Overactive bladder
Adult: Initially, 7.5 mg once daily, may be increased to 15 mg once daily after at least 2 weeks in patients requiring greater symptom relief according to individual response.
|
Indications and Dosage
Oral
Overactive bladder Adult: Initially, 7.5 mg once daily, may be increased to 15 mg once daily after at least 2 weeks in patients requiring greater symptom relief according to individual response.
|
|
Special Patient Group
Patients taking potent CYP2D6 inhibitors (e.g. paroxetine, terbinafine, quinidine, cimetidine), or moderate CYP3A4 inhibitors (e.g. fluconazole, erythromycin, grapefruit juice): Initially, 7.5 mg daily, may be titrated to 15 mg daily according to clinical response and individual tolerability.
Patients taking potent CYP3A4 inhibitors e.g. ketoconazole, itraconazole, ritonavir: Max 7.5 mg daily. Pharmacogenomics Darifenacin is extensively metabolised into inactive metabolites by CYP3A4 and CYP2D6 isoenzymes. It affects variability on pharmacokinetics to individuals who lack CYP2D6 enzyme activity, known as CYP2D6 poor metabolisers, may experience increased darifenacin exposure since the metabolism in these people will be principally mediated by CYP3A4 isoenzyme. The prevalence of CYP2D6 poor metabolisers is estimated at approx 7% in Caucasians and 2% in African Americans. EMA and FDA approved drug labels for Darifenacin cited that CYP2D6 poor metaboliser may experience increased darifenacin Max plasma concentrations and exposure as compared to CYP2D extensive metabolisers. However, no dosage adjustment has been recommended for specific CYP2D6 genotypes according to currently available professional society practice guidelines. |
|
Hepatic Impairment
Moderate (Child-Pugh class B): Max: 7.5 mg daily. Severe (Child-Pugh C): Contraindicated.
|
|
Administration
May be taken with or without food. Swallow whole, do not chew/crush/divide.
|
|
Contraindications
Urinary retention, gastric retention, uncontrolled narrow-angle glaucoma, myasthenia gravis, severe ulcerative colitis, toxic megacolon. Severe hepatic impairment.
|
|
Special Precautions
Patients with autonomic neuropathy, hiatus hernia, controlled or treated narrow-angle glaucoma, pre-existing cardiac diseases, GERD, decreased gastrointestinal motility (e.g. severe constipation, ulcerative colitis), gastrointestinal obstructive disorders (e.g. pyloric stenosis), bladder flow obstruction, prostate enlargement, risk for urinary retention. Caution during hot weather conditions and exercise. Concomitant use with potent CYP2D6 and moderate CYP3A4 inhibitors. Renal and mild to moderate hepatic impairment. Pregnancy and lactation. CYP2D6 poor metabolisers.
|
|
Adverse Reactions
Significant: Acute urinary retention, severe constipation, CNS effects (e.g. headache, confusion, hallucination, somnolence), heat prostration (during hot environment).
Eye disorders: Dry eyes, visual disturbance, blurred vision. Gastrointestinal disorders: Dry mouth, constipation, nausea, abdominal pain, dyspepsia flatulence, diarrhoea, mouth ulceration, altered taste. General disorders and admin site conditions: Asthenia, peripheral/face oedema. Investigations: Increased AST/ALT, weight gain. Nervous system disorders: Dizziness. Psychiatric disorders: Insomnia, abnormal thinking. Renal and urinary disorders: Urinary tract disorder, bladder pain, UTI. Reproductive system and breast disorders: Erectile dysfunction, vaginitis. Respiratory, thoracic and mediastinal disorders: Nasal dryness, dyspnoea, cough, rhinitis, flu symptoms. Skin and subcutaneous tissue disorders: Rash, dry skin, pruritus, hyperhidrosis. Vascular disorders: Hypertension. Potentially Fatal: Angioedema of the face, lips, tongue or larynx. |
|
Patient Counseling Information
This drug may cause dizziness, somnolence, blurred vision or insomnia, if affected, do not drive or operate machinery.
|
|
Monitoring Parameters
Monitor LFTs and for signs or symptoms of anticholinergic effects (e.g. confusion, headache, tremors) and hypersensitivity reactions.
|
|
Overdosage
Symptoms: Dry mouth, constipation, headache, dyspepsia, abnormal vision, nasal dryness, and severe antimuscarinic effects. Management: Symptomatic and supportive treatment. May administer physostigmine to reverse symptoms and ECG monitoring.
|
|
Drug Interactions
May exacerbate oesophagitis with oral bisphosphonates. Increased exposure with potent CYP2D6 inhibitors (e.g. paroxetine, terbinafine, cimetidine, quinidine), and moderate CYP3A4 inhibitors (e.g. erythromycin, clarithromycin, fluconazole). Decreased plasma concentrations with CYP3A4 inducers (e.g. rifampicin, carbamazepine, barbiturates). May increase exposures of midazolam and digoxin. Increased risk of adverse effects with other antimuscarinic agents (e.g. oxybutynin, tolterodine, flavoxate). Increased plasma concentrations of CYP2D6 substrates with narrow therapeutic index (e.g. flecainide, TCAs, thioridazine). Significantly increased exposure with potent CYP3A4 inhibitors (e.g. protease inhibitors, ketoconazole, itraconazole) and potent P-glycoprotein inhibitors (e.g. ciclosporin, verapamil).
|
|
Food Interaction
Increased exposure with grapefruit or grapefruit juice. Decreased plasma concentrations with St. John’s wort.
|
|
Action
Description:
Mechanism of Action: Darifenacin selectively antagonises the muscarinic (cholinergic) M3 subtype receptors which controls the urinary bladder muscle contraction, thereby reducing symptoms of bladder irritability or overactivity e.g. urge incontinence, urgency and frequency. Pharmacokinetics: Absorption: Rapidly and completely absorbed from the gastrointestinal tract. Bioavailability: Approx 15-19%. Time to peak plasma concentration: Approx 7 hours. Distribution: Volume of distribution: Approx 163 L. Plasma protein binding: Approx 98%, mainly to α1-acid glycoprotein. Metabolism: Undergoes extensive first-pass metabolism in the liver via monohydroxylation in the dihydrobenzofuran ring, dihydrobenzofuran ring opening, and N-dealkylation of the pyrrolidine nitrogen by CYP3A4 and CYP2D6 isoenzymes to inactive metabolites. Excretion: Via urine (approx 60%) and faeces (40%), as inactive metabolites. Elimination half-life: Approx 13-19 hours. |
|
Chemical Structure
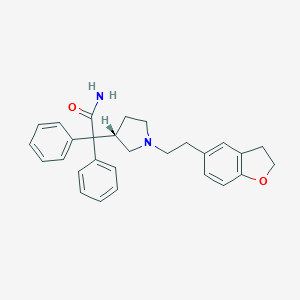 Source: National Center for Biotechnology Information. PubChem Database. Darifenacin, CID=444031, https://pubchem.ncbi.nlm.nih.gov/compound/Darifenacin (accessed on Jan. 20, 2020) |
|
Storage
Store at 25°C. Protect from light.
|
|
ATC Classification
G04BD10 - darifenacin ; Belongs to the class of urinary antispasmodics.
|
|
References
Annotation of EMA Label for Darifenacin and CYP2D6. Pharmacogenomics Knowledgebase (PharmGKB). https://www.pharmgkb.org/. Accessed 02/10/2019. Annotation of FDA Label for Darifenacin and CYP2D6. Pharmacogenomics Knowledgebase (PharmGKB). https://www.pharmgkb.org/. Accessed 02/10/2019. Annotation of HCSC Label for Darifenacin and CYP2D6. Pharmacogenomics Knowledgebase (PharmGKB). https://www.pharmgkb.org/. Accessed 02/10/2019. Anon. CYP2D6 - Darifenacin (Pharmacogenomics). Lexicomp Online. Hudson, Ohio. Wolters Kluwer Clinical Drug Information, Inc. https://online.lexi.com. Accessed 02/10/2019. Anon. Darifenacin. AHFS Clinical Drug Information [online]. Bethesda, MD. American Society of Health-System Pharmacists, Inc. https://www.ahfscdi.com. Accessed 02/10/2019. Anon. Darifenacin. Lexicomp Online. Hudson, Ohio. Wolters Kluwer Clinical Drug Information, Inc. https://online.lexi.com. Accessed 02/10/2019. Buckingham R (ed). Darifenacin. Martindale: The Complete Drug Reference [online]. London. Pharmaceutical Press. https://www.medicinescomplete.com . Accessed 02/10/2019. Darifenacin Tablet, Extended Release (Cipla USA Inc). DailyMed. Source: U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/. Accessed 04/10/2016. Enablex Tablet, Extended Release (Allergan, Inc). DailyMed. Source: U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed/. Accessed 02/10/2019. Joint Formulary Committee. Darifenacin. British National Formulary [online]. London. BMJ Group and Pharmaceutical Press. https://www.medicinescomplete.com. Accessed 02/10/2019.
|