Acute migraine attacks
Adult: For cases with or without aura: 2.5 mg as soon as possible after onset of attack; may repeat the dose after at least 2 hours if symptoms recur after an initial response. Max: 5 mg daily.
|
Indications and Dosage
Oral
Acute migraine attacks Adult: For cases with or without aura: 2.5 mg as soon as possible after onset of attack; may repeat the dose after at least 2 hours if symptoms recur after an initial response. Max: 5 mg daily.
|
|
Hepatic Impairment
Severe (Child-Pugh class C): Contraindicated.
|
|
Administration
May be taken with or without food. Take on an empty stomach for fast relief.
|
|
Contraindications
Hypersensitivity. History of MI; ischaemic heart disease, coronary vasospasm (e.g. Prinzmetal's angina), peripheral vascular disease, signs or symptoms compatible with ischaemic heart disease, moderately severe or severe hypertension; uncontrolled mild hypertension, history of CVA or TIA, Wolff-Parkinson-White syndrome or arrhythmias associated with other cardiac accessory conduction pathway disorders, history of hemiplegic or basilar migraine; ischaemic bowel disease. Severe hepatic impairment (Child-Pugh class C). Concomitant use with or within 24 hours of taking ergotamine or ergotamine derivatives (including methysergide, dihydroergotamine) or other 5-hydroxytryptamine (5-HT1) receptor agonists.
|
|
Special Precautions
Patient with risk factors for CAD (e.g. diabetes, hypercholesterolaemia, strong family history of CAD, controlled hypertension, postmenopausal women, males >40 years, obesity, smoking). Not indicated for the treatment of hemiplegic, basilar, or ophthalmoplegic migraine, cluster headache, or for prophylaxis of migraine. Elderly. Pregnancy and lactation.
|
|
Adverse Reactions
Significant: Sensation of pain, tightness, heaviness, and pressure in the chest, neck, throat, and jaw; non-coronary vasospastic reactions (e.g. gastrointestinal vascular ischaemia and infarction, peripheral vascular ischaemia, splenic infarction, Raynaud's syndrome), transient or permanent blindness, partial vision loss; medication overuse headache (prolonged-use). Rarely, significant blood pressure elevation (including hypertensive crisis with acute impairment of organ systems).
Gastrointestinal disorders: Abdominal pain, dyspepsia, dry mouth, nausea. General disorders and administration site conditions: Fatigue. Nervous system disorders: Headache, dizziness, somnolence, paraesthesia, dysaesthesia, hypoaesthesia. Skin and subcutaneous tissue disorders: Hyperhidrosis. Vascular disorders: Flushing. Potentially Fatal: Cerebrovascular events (e.g. subarachnoid or cerebral haemorrhage, stroke); anaphylaxis, anaphylactoid, hypersensitivity reaction (e.g. angioedema); serotonin syndrome. Rarely, serious cardiac events (e.g. MI, Prinzmetal's angina, ventricular tachycardia, ventricular fibrillation, cardiac arrest). |
|
Patient Counseling Information
This drug may cause drowsiness, dizziness or weakness, if affected, do not drive or operate machinery.
|
|
Monitoring Parameters
Monitor blood pressure, CV status (periodically), and headache severity. Obtain ECG during 1st dose administration and periodically in patients with multiple CV risk factors who have a negative CV evaluation. Perform CV evaluation prior to initiation of therapy in patients with multiple CV risk factors. Monitor signs and symptoms suggestive of angina, serotonin syndrome, and hypersensitivity reactions.
|
|
Drug Interactions
May increase the risk of hypertension, or coronary vasoconstriction with SSRIs (e.g. paroxetine, sertraline, citalopram, fluvoxamine, fluoxetine). May increase the risk of coronary artery constriction and hypertension with methylergometrine. Increased serum concentrations with fluvoxamine, propranolol, and oral contraceptives.
Potentially Fatal: Increased risk of hypertension and coronary artery constriction due to additive vasoconstricting effect with ergotamine, ergotamine derivatives (including methysergide), and other 5-HT1 receptor agonists. Increased risk of serotonin syndrome with MAOIs, TCAs, SNRIs, SSRIs and buprenorphine. |
|
Food Interaction
Increased risk of serotonin syndrome with St. John's wort.
|
|
Action
Description:
Mechanism of Action: Frovatriptan is a selective agonist for serotonin (5-HT1B and 5-HT1D receptors) in cranial arteries. It relieves migraine by causing vasoconstriction and decreasing the sterile inflammation associated with antidromic neuronal transmission. Pharmacokinetics: Absorption: Incompletely absorbed from the gastrointestinal tract. Bioavailability: Approx 20% (male); approx 30% (female). Time to peak plasma concentration: 2-4 hours. Distribution: Distributes into cellular fraction of blood, principally erythrocytes. Plasma protein binding: Approx 15%. Metabolism: Metabolised in the liver by CYP1A2 isoenzyme. Excretion: Via faeces (62%); urine (32%). Elimination half-life: Approx 26 hours. |
|
Chemical Structure
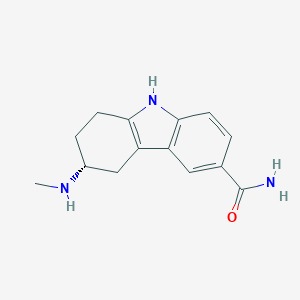 Source: National Center for Biotechnology Information. PubChem Compound Summary for CID 77992, Frovatriptan. https://pubchem.ncbi.nlm.nih.gov/compound/Frovatriptan. Accessed Nov. 24, 2022. |
|
Storage
Store between 15-30°C. Protect from moisture.
|
|
MIMS Class
|
|
ATC Classification
N02CC07 - frovatriptan ; Belongs to the class of selective serotonin (5HT1) agonists preparations. Used to relieve migraine.
|
|
References
Anon. Frovatriptan. AHFS Clinical Drug Information [online]. Bethesda, MD. American Society of Health-System Pharmacists, Inc. https://www.ahfscdi.com. Accessed 07/11/2022. Anon. Frovatriptan. Lexicomp Online. Hudson, Ohio. Wolters Kluwer Clinical Drug Information, Inc. https://online.lexi.com. Accessed 07/11/2022. Buckingham R (ed). Frovatriptan. Martindale: The Complete Drug Reference [online]. London. Pharmaceutical Press. https://www.medicinescomplete.com. Accessed 07/11/2022. Frovatriptan Tablet, Film Coated (Ingenus Pharmaceuticals, LLC). DailyMed. Source: U.S. National Library of Medicine. https://dailymed.nlm.nih.gov/dailymed. Accessed 07/11/2022. Joint Formulary Committee. Frovatriptan. British National Formulary [online]. London. BMJ Group and Pharmaceutical Press. https://www.medicinescomplete.com. Accessed 07/11/2022. Mylatrip 2.5 mg Film-coated Tablets (Generics [UK] Ltd. t/a Mylan). MHRA. https://products.mhra.gov.uk. Accessed 07/11/2022.
|